
Decoda Health launched on Y Combinator's "Launch YC" recently!
Decoda Health leverages AI to read electronic health record systems to automatically assign billing codes to clinician notes. The result? Clinics save 30% in coding costs, see 20% fewer claim denials, and cut claim processing time from days to seconds.
Founded by Daniyal Afzal & Kevin Cheng, two mathematicians who are passionate about creating impactful software. Daniyal worked in the fintech industry, while Kevin developed machine learning software for a high-growth radiology-tech startup. Their experiences in high-growth medical imaging & fintech industries worldwide have given them unique insights into the intersection of AI, healthcare, and finance.
From their experiences, they realized that the fundamental language through which money flows in healthcare is designed to be error-prone. This became particularly evident when Daniyal's father, a general surgeon, was scammed out of many months’ wages as his employer consistently claimed their cash flows were stuck with an insurer. Consequently, healthcare's lack of financial transparency frustrated him and his colleagues. Drawn by a desire to rectify the situation, the founders decided to address the problem of medical coding.
Medical coding is the language connecting the world of healthcare providers with that of insurance companies. At its core, medical coding is a vital process that translates healthcare diagnoses, procedures, medical services, and equipment into universal medical alphanumeric codes.
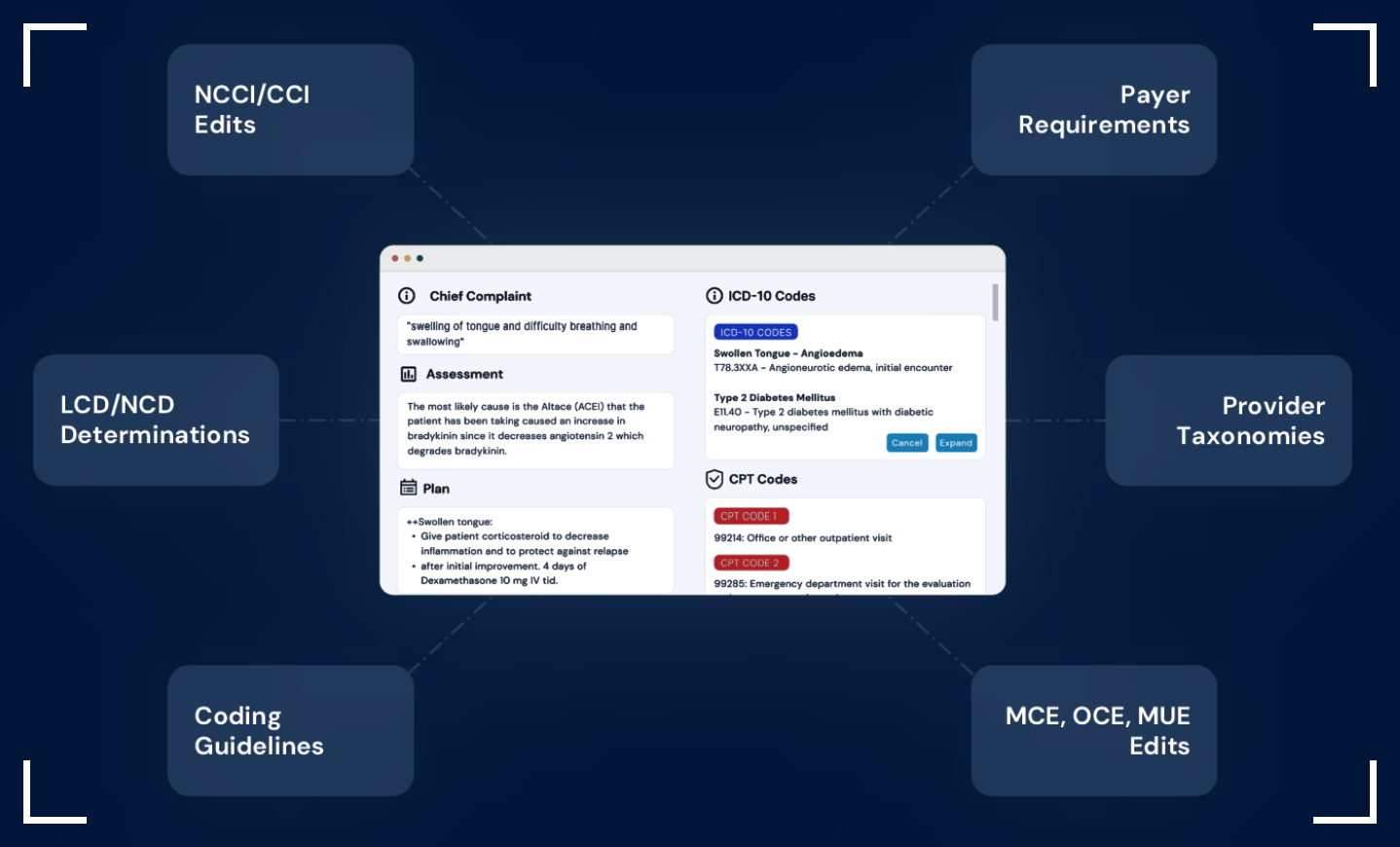
Insurers base their payments on the accuracy of how these medical codes are assigned. The guidelines governing what is considered accurate evolve all the time & doctors don't have the time to keep up with all of this. Doctors attend medical school to treat patients, not to navigate complex coding rulesets for insurers. But this is what they ought to do to get paid.
This process is predominantly handled by human coders manually reviewing medical documentation and assigning appropriate codes by checking payer guidelines and coding rulesets. Given the manual approach and constantly evolving requirements, care providers must deal with coding backlogs, coding errors, delayed reimbursements, and increased administrative costs.
Annually, a colossal $20B is spent on this complex coding process today. Practices often recover as little as 60% of what they bill, with some even spending up to 15% of their claims volume on third-party processing fees. This resource drain significantly elevates the cost of care, causing a domino effect on the entire healthcare system.
With a lack of certified talent & an aging workforce, there is a growing need for good software to fill this gap.
Decoda Health can serve the market's accuracy and talent supply gap with fully autonomous medical coding & billing software that is designed to be -
