Founded by Tej Seelamsetty & Aumesh Misra - great friends from college who:
Tej – Ran growth (10x-ed revenue) at Fair Square (W20) and was an AC at Bain. Paid for college by flipping houses. Studied CS at WashU.
Aumesh – Ex-Microsoft and was the 8th engineer at Compound (S19). Built medical imaging software used by Stanford. Also studied CS at WashU.
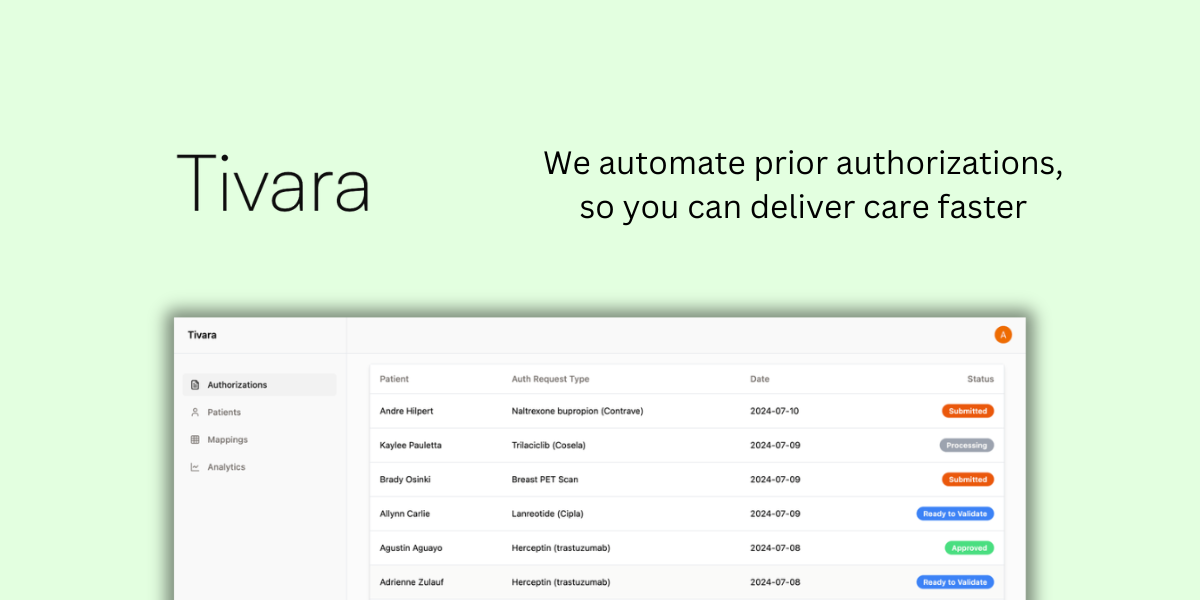
Tivara’s mission is to help doctors deliver care to patients faster. They’re starting by using LLMs to automate submitting prior authorization requests (and getting their approval) on behalf of providers.
Prior authorization is a process by which physicians must justify their treatment plan of a patient to that patient’s health insurance carrier as “medically necessary.”
Right now, medical groups employ a team (1 employee focused on prior authorizations per 1-5 physicians) to handle this process with insurance carriers manually. These teams are frequently operating over capacity; some of the practices are so backlogged that a request isn’t even submitted until up to a week after a doctor’s order is placed.
Figure 1: 94% of Physicians Report Delayed Patient Care due to Prior Authorization (Source: American Medical Association Survey of 1,000 Doctors.

As you can imagine, insurance carriers are incentivized to delay and/or deny approval as much as they can. Some carriers are so egregious that they’re incurring fines in the tens of millions for morbidly delaying the care of sick patients. A patient who is exhibiting signs of colon cancer definitely shouldn’t have to wait months (or even days) for a colonoscopy.
At the end of the day, Tivara does two things:
